Shining a light on TK2d
Thymidine kinase 2 deficiency (TK2d) is a rare, inherited, debilitating, and often fatal myopathic mitochondrial disease.1,2 It is also a mitochondrial depletion and deletion syndrome, a category of mitochondrial disease.3
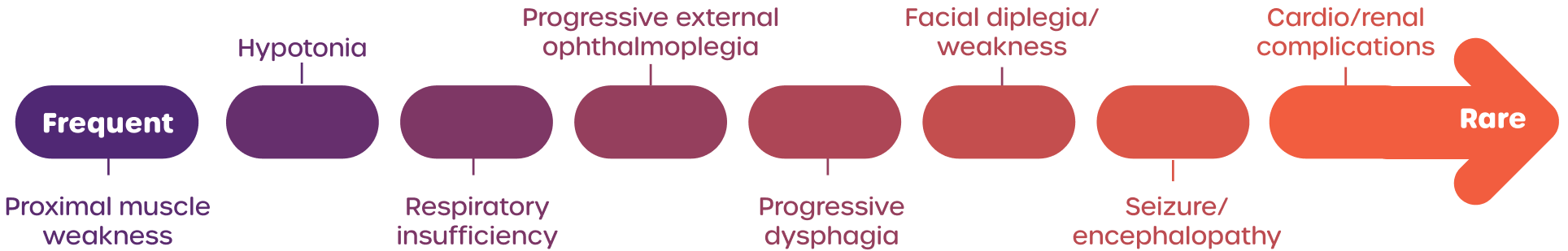
TK2d is a primary mitochondrial myopathy that is different from other mitochondrial diseases in that it predominantly manifests as muscle weakness.1
This proximal muscle weakness affects different parts of the body. Patients may lose the ability to walk, eat, and breathe independently.1,4,5
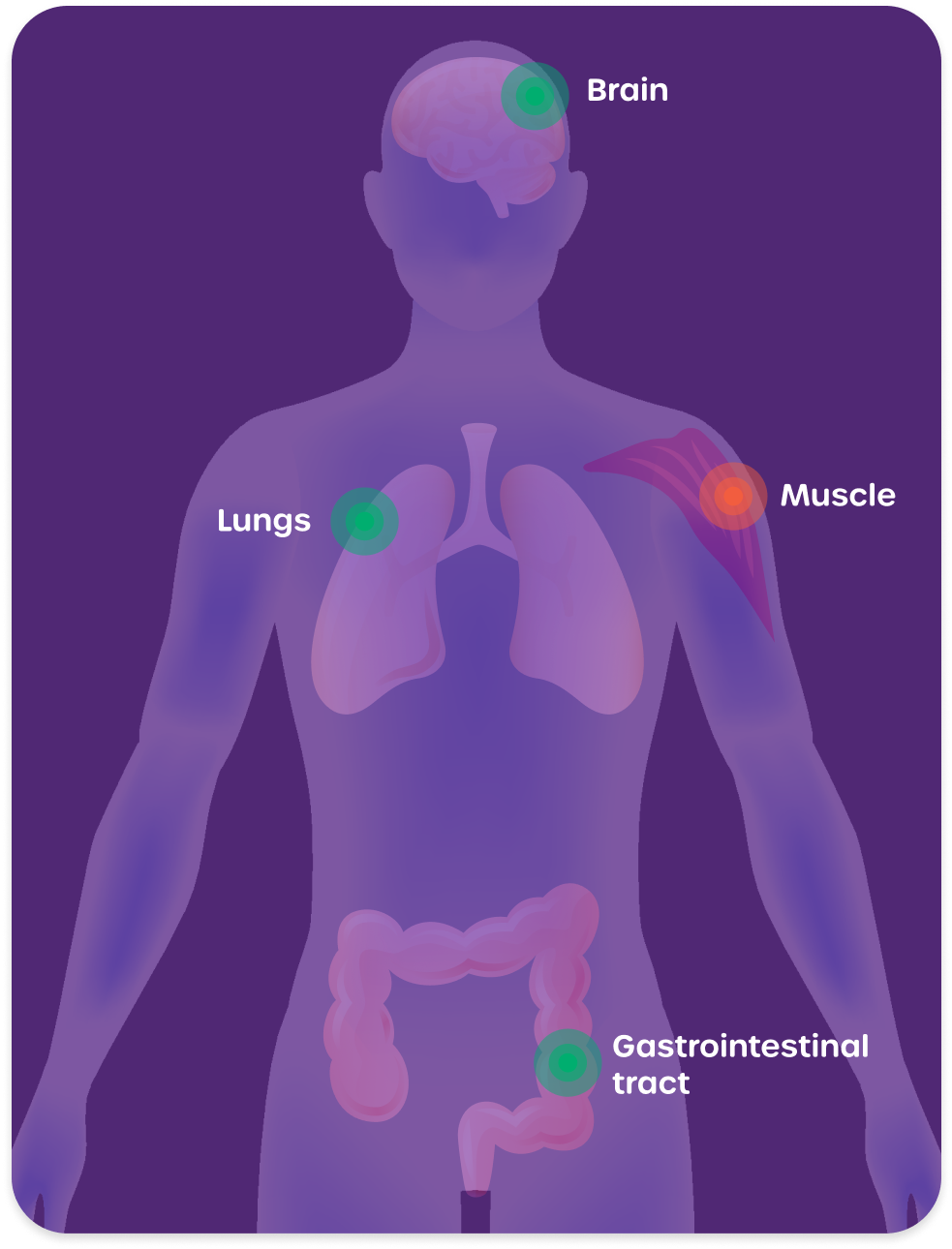
Organ system and related symptoms1,3-5:
TK2d is often fatal.
When age of symptom onset is 1 year and younger, survival is less than 1 year.4,5
TK2d is a deficiency of the thymidine kinase 2 enzyme, which is crucial for the maintenance and synthesis of mitochondrial DNA (mtDNA).4,6
TK2d is a result of a defect in a nuclear gene (in this case, the TK2 gene), whereas many other mitochondrial diseases are caused by defects in mitochondrial genes.6,7
TK2d can develop at any point in a patient’s life5
Early onset of TK2d is related to more severe symptoms with a faster disease progression. Late onset of TK2d may be possible and is defined as symptom onset after 12 years.4,5
Because long diagnostic journeys and misdiagnoses are common for patients with mitochondrial diseases, people with TK2d may be diagnosed years after symptom onset. Even those diagnosed as adults may have early-onset TK2d if their symptoms began at or before 12 years of age.3,6,8
Early onset of TK2d1,4,5
Onset from 0-12 years
Infants often have a healthy birth and reach early developmental milestones.
Shortly after, they may experience rapid decline characterized by loss of motor milestones and acute respiratory insufficiency.
Patients with disease onset between ages 1 and 12 years have a median post-onset survival to at least 13 years, but this number decreases when onset happens at an earlier age. Infants with symptom onset before age 1 have a median post-onset survival of approximately 1 year.
Manifestations include facial weakness, droopy eyelids, difficulty eating, shortness of breath, and proximal muscle weakness.1,5
Early onset of TK2d can be divided into 2 subgroups1,3-5,9
Infantile onset (onset ≤1 year)
- Often a healthy birth
- Early growth and development is normal
- Symptom onset is followed by rapid decline
- Median post-onset survival is approximately 1 year
Childhood onset (onset >1 and ≤12 years)
- Disease progression varies between patients
- Children may lose motor milestones
- Many patients require mobility and ventilatory support
- Median post-onset survival is to at least 13 years

TK2d may make my body weaker at certain things, but all that means is that I need different types of support than others.
Connie, lives with TK2d

only certain genetic tests can definitively confirm a diagnosis1,5
That means some patients may need further genetic testing.10
The TK2 gene is found in the nuclear genome, not the mitochondrial genome.6
Because not all tests include the nuclear genome, many do not look for TK2d. Whole-exome sequencing, whole-genome sequencing, and broad genetic panels for nuclear mitochondrial genes usually include TK2.
Order these genetic tests to definitively diagnose TK2d.1,5
View Resources
Discover various resources regarding TK2d, mitochondrial diseases, and more
- Thymidine kinase 2 deficiency. National Organization for Rare Disorders. Updated March 4, 2025. Accessed March 24, 2025. https://rarediseases.org/rare-diseases/thymidine-kinase-2-deficiency/
- Domínguez-González C, Madruga-Garrido M, Hirano M, et al. Collaborative model for diagnosis and treatment of very rare diseases: experience in Spain with thymidine kinase 2 deficiency. Orphanet J Rare Dis. 2021;16(1):407. doi:10.1186/s13023-021-02030‑w
- Berardo A, Domínguez-González C, Engelstad K, et al. Advances in thymidine kinase 2 deficiency: clinical aspects, translational progress, and emerging therapies. J Neuromuscul Dis. 2022;9(2):225–235. doi:10.3233/JND-210786
- Garone C, Taylor RW, Nascimento A, et al. Retrospective natural history of thymidine kinase 2 deficiency. J Med Genet. 2018;55(8):515–521. doi:10.1136/jmedgenet-2017-105012
- Wang J, El-Hattab AW, Wong LJC. TK2-Related Mitochondrial DNA Maintenance Defect, Myopathic Form. In: Adam MP, Feldman J, Mirzaa GM, et al, eds. GeneReviews®. [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2024.
- Domínguez-González C, Hernandez-Lain A, Rivas E, et al. Late-onset thymidine kinase 2 deficiency: a review of 18 cases. Orphanet J Rare Dis. 2019;14(1):1–10. doi:10.1186/s13023-019-1071‑z
- Parikh S, Goldstein A, Koenig MK, et al. Diagnosis and management of mitochondrial disease: a consensus statement from the Mitochondrial Medicine Society. Genet Med. 2015;17(9):689–701. doi:10.1038/gim.2014.177
- Grier J, Hirano M, Karaa A, et al. Diagnostic odyssey of patients with mitochondrial disease: results of a survey. Neurol Genet. 2018;4(2):e230. doi:10.1212/NXG.0000000000000230
- Kaler J, Hussain A, Patel S, Majhi S. Neuromuscular junction disorders and floppy infant syndrome: a comprehensive review. Cureus. 2020;12(2):e6922. doi:10.7759/cureus.6922
- Nicolau S, Milone M, Liewluck T. Guidelines for genetic testing of muscle and neuromuscular junction disorders. Muscle Nerve. 2021;64(3):255-269. doi:10.1002/mus.27337